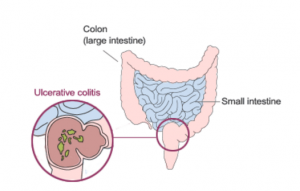
Ulcerative Colitis and Proctitis
What Is Ulcerative Colitis?
Ulcerative colitis is a chronic disease of the colon (large intestine). The disease is marked by inflammation and ulceration of the colon lining which makes the colon empty frequently. Symptoms include diarrhea (sometimes bloody) and often crampy abdominal pain. The inflammation usually begins in the rectum and lower colon, but it may also involve the entire colon. When ulcerative colitis affects only the rectum, it is called ulcerative proctitis.
Ulcerative colitis differs from Crohn’s disease. Both diseases are called inflammatory bowel disease (IBD). Crohn’s disease can affect any part of the GI tract, whereas ulcerative colitis affects only the colon. The inflammation affects only the innermost lining of the colon, but in Crohn’s disease, it can affect the entire thickness. Inflammation from ulcerative colitis occurs in a continuous process – there are no areas of normal intestine between the areas of the diseased intestine. In contrast, “skip” areas may occur in Crohn’s disease.
What Are The Causes of Ulcerative Colitis?
We do not yet know what causes this disease. Studies indicate that the inflammation in ulcerative colitis involves a complex interaction of factors: the genes the person has inherited, the immune system, and something in the environment. Foreign substances (antigens) in the environment may be the direct cause of the inflammation, or they may stimulate the body’s defenses to produce an inflammation that continues without control. In patients with ulcerative colitis, once the patient’s immune system is “turned on,” it does not know how to properly “turn off.” As a result, inflammation damages the intestine and causes the symptoms of ulcerative colitis. One of the major goals of medical therapy is to help patients to better regulate their immune system.
What Are The Signs And Symptoms of Ulcerative Colitis?
Symptoms of ulcerative colitis include diarrhea (often bloody) which may be associated with crampy abdominal pain and sudden urgency to have a bowel movement. Diarrhea may begin slowly or quite suddenly. Loss of appetite, weight loss, and fatigue are also common symptoms. In cases of severe bleeding, anemia may occur. Approximately half of all patients with ulcerative colitis have relatively mild symptoms. The symptoms of ulcerative colitis tend to come and go, with fairly long periods in between flare-ups in which patients may experience no distress at all. These periods of remission can span months or even years, although symptoms do eventually return. Of note is that the disease is not always limited to the GI tract; it can also affect the joints, eyes, skin, and liver.
What Are The Risk Factors of Ulcerative Colitis?
It is estimated that as many as one million Americans have IBD — with that number evenly split between Crohn’s disease and ulcerative colitis. Males and females appear to be affected equally. The usual age of diagnosis with ulcerative colitis is in the mid-30’s, although the disease can occur at any age. Men are more likely than women to be diagnosed with ulcerative colitis in their 50s and 60s. The incidence is greater in whites than non-whites, and a higher incidence is found in Jews than in non-Jews.
IBD tends to run in families. Studies have shown that up to 20 percent of patients with ulcerative colitis will have a close relative with either Crohn’s disease or ulcerative colitis. There is no way to predict which, if any, family members will develop ulcerative colitis.
How is Ulcerative Colitis Diagnosed?
The diagnosis of ulcerative colitis is based on the patient’s clinical history, a physical exam and a series of tests which usually includes: stool studies, blood tests, and a colonoscopy. Doctors rely on a combination of the patient’s history and physical exam, results of laboratory tests, X-rays (small bowel series), colonoscopy and recently, small bowel capsule endoscopy.
What Are Possible Treatments For Ulcerative Colitis?
Medications Used To Treat Ulcerative Colitis
Currently, there is no cure for ulcerative colitis. The goal of medical treatment, therefore, is to modulate the inflammatory response. Several groups of drugs are used to treat ulcerative colitis. They are:
-
- Aminosalicylates (5-ASA): These medications typically are used to treat mild to moderate symptoms.
- Corticosteroids: These drugs have significant short and long-term side effects and should not be used as a maintenance medication.
- Immune modifiers: Azathioprine (Imuran®), 6-MP (Purinethol®), and methotrexate are used to help decrease corticosteroid dosage and also to help heal fistulas. In addition, immune modifiers can help maintain disease remission.
- Antibiotics: metronidazole, ciprofloxacin, ampicillin, others.
- Biologic therapies. Infliximab (Remicade®). Infliximab is used for people with moderate-to-severe ulcerative colitis.
Role of Surgery
In one-quarter to one-third of patients with ulcerative colitis, medical therapy is not completely successful or complications arise. Under these circumstances, surgery may be considered. This operation involves the removal of the colon (colectomy). Ulcerative colitis is “cured” once the colon is removed.
Steps To Help With Ulcerative Colitis and Proctitis
Nutrition
There is no evidence that any particular foods cause or contribute to ulcerative colitis. Paying special attention to diet may help reduce symptoms, replace lost nutrients, and promote healing. Maintaining proper nutrition is important for the medical management of ulcerative colitis.
Except for restricting milk in lactose-intolerant patients, or restricting coffee when severe diarrhea occurs, most gastroenterologists recommend a well-balanced diet. A healthy diet should contain a variety of foods from all food groups. Meat, fish, poultry, and dairy products (if tolerated) are sources of protein; bread, cereal, starches, fruits, and vegetables are sources of carbohydrate; margarine and oils are sources of fat.
Emotional Factors
There is no evidence to show that stress, anxiety, or tension is responsible for ulcerative colitis. However, they may contribute to an exacerbation of the disease. The emotional distress that patients sometimes feel may be a reaction to the symptoms of the disease itself. Although formal psychotherapy is generally not necessary, some patients are helped considerably by speaking with a therapist who is knowledgeable about IBD or about chronic illness in general.